The number of implants placed by dentists and dental specialists is increasing based on a predictable outcome of success. A comprehensive treatment plan includes advising the patient of the risk of failure based on smoking, history of radiotherapy, systemic health issues, and local bone quality and quantity. Peri-implant disease is a combination of poor oral hygiene, placement of a non-cleansable prosthetic, or recommendations that are not effective for implants. Thus, one of the key factors to implant success is the adherence to an effective maintenance program to ensure longevity of the implant.10
Dental hygienists play an intricate role in the overall success of dental implants. With the placement of dental implants becoming more common, it is important for hygienists to have a protocol for maintenance. The following is a review of recent studies with information regarding dental implants and proper maintenance.

Implant Failure
Dental implants yield excellent long-term results with 10-year success and survival rates above 95%.7 The reasons for implant failure are still being studied. A thorough medical history is imperative to weigh risk factors of implant failure. Smoking and radiotherapy have been shown to increase implant failure. Studies have shown diabetes and osteoporosis are also risk factors, though more thorough studies are needed to confirm an association.
Other risk factors include biomechanical overload as well as infection and inflammation. Patients with poorly controlled diabetes suffer from impaired osseointegration, elevated risk of peri-implantitis, and a higher level of implant failure. The influence of duration of the disease is not fully clear. When diabetes is well controlled, implant procedures are safe and predictable with a complication rate like that of healthy patients.1 Always get the patients most recent hbA1c reading, current perio chart to help assess inflammation, smoking history, and history of osteoporosis before implant surgery. With this information, the doctor can better discuss the risk factors of implant failure.
Instrumentation
The impact of scalers on implant abutment surfaces varies between abutment types, presumably due to different surface characteristics, with no apparent advantage of one abutment type over the other with regard to resistance to surface damage. Unfilled resin was found consistently to be the least damaging to abutment surfaces, although all scalers of all compositions caused detectable surface changes to polished surfaces of implant abutments.
A study conducted in 2014 compared cleaning effectiveness of implant prophylaxis instruments. Instrument types included in the study were a plastic curette, carbon-fiber reinforced plastic curette, a sonic driven device with prophylaxis brush without prophylaxis paste, rotating rubber cup with prophylaxis paste, sonic driven device with a plastic instrument tip, ultrasonic device with a plastic instrument tip, and air polishing using low abrasive amino acid (glycine) powder. Nearly all instruments inflicted at least slight damage such as scratches or rounded edges on surface structure. The best cleaning effectiveness was observed with the sonic and ultrasonic oscillating plastic tips and air polishing. Second most effective was the prophylactic brush and prophylactic cup. The least effective was the manual plastic, and carbon-fiber reinforced plastic curettes.

Suggested Maintenance Protocol
Soft tissue assessment: The soft-tissue assessment includes checking for visual signs of gingival inflammation, such as redness, swelling, alterations of contour and consistency, aberrant gingival form or the presence of fistulas.6
Plaque index: It is recommended that some objective form of plaque monitoring be performed and documented at every maintenance visit, to allow longitudinal assessment of oral hygiene.
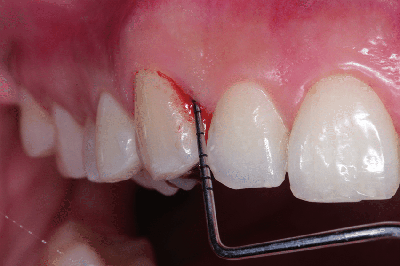
Clinical probing depth: Probing is an important and reliable diagnostic parameter in long-term monitoring of all soft tissues including peri-implant soft tissues. The safety of probing around implant restorations has been well-established, and this procedure does not seem to jeopardize the integrity of oral implants.6 However, less probing force is needed around implants due to the decreased attachment strength to the implant and the connective tissue. It is recommended to wait at least three months after placement before probing implants.

Bleeding on probing: A study of implants confirmed that absence of bleeding on probing was an accurate indication of stability.6 It has been reported that bleeding on probing alone yields higher diagnostic accuracy at implant sites compared with natural tooth sites.10These studies highlight the importance of recording bleeding on probing when performing periodontal evaluation to monitor peri-implant soft tissues.
Suppuration: Suppuration should be noted. Suppuration has been associated with peri-implantitis and can be an indicator that anti-infective therapy is warranted.6,10
Stability of the soft tissue margins: Though a correlation between implant failure and stability of soft tissue around implants has not been established, it is important to evaluate and take note of any apical migration of the tissue. Recession can expose rough implant structures, which accumulate more plaque and could lead to inflammation and possible peri-implant mucositis.6
Occlusion: Studies indicate there is a direct correlation between occlusal overload and peri-implant bone loss. Occlusion should be checked at regular intervals to identify and occlusal disharmonies. Premature contacts or other interferences should be identified and corrected.9 A case report published in the International Journal of Oral & Maxillofacial Implants found that “The placement of an unstable removable prosthesis on three well-integrated implants that had been stable for nine years caused noticeable bone loss after six months. The elimination of the traumatic occlusion reversed the situation. The condition has been stable for the past four years”11
Radiographs to monitor bone level: Preservation of crestal bone height is crucial to the long-term success of an implant. Radiographs to monitor crestal bone loss is recommended. To establish baseline bone levels, a radiograph should be taken at implant placement, and again at prosthesis insertion.6 A periapical/vertical bitewing radiograph should be taken at 6-8-month intervals and compared to the baseline to assess crestal bone. If the bone level is stable another periapical/vertical bitewing should be taken after one year and compared. If the bone level continues to be stable periapical/vertical bitewing should be taken every three years. However, any time crestal bone levels change, radiographs should be taken and reviewed every 6-8 months until the bone level is stable for two consecutive periods.10


