When it comes to evolution, our profession is in a constant state of flux. There are lots of things I love about my work here at Dental Products Report and one of those things is that I get the chance to bring information about the latest improvements to my peers. With the exponential increase in research and development, along with manufacturing capabilities, the art and science of dentistry now exists as a “moving sidewalk” that requires practitioners to put in effort to constantly move forward or risk moving backward.
Along those lines, in the time that I’ve been practicing, I can say with confidence that there’s not one single thing I do routinely that was state of the art when I was trained. Even for recent graduates, this can be a challenge. First, they’ve got to spin up on the latest evolutions that weren’t taught in dental school, then they have to make sure they stay up to date with the constant changes. It’s the equivalent of jumping onto a moving train and then trying desperately to hang on.
For those who’ve been practicing a while, you must not become stuck in a rut of your own making. The challenge of our profession is to always be the very best you can be, every day. That means keeping an open mind and expanding your skill sets with the latest innovations that can provide state-of-the-art patient outcomes.
For this article, let’s take a look at some things that can help decrease the stresses faced by doctors and patients in daily practice.
* Injections
Do you happen to know even one person who likes either giving or receiving a dental injection? Me neither. Of all the things we do, it’s probably the least liked and most likely creates more stress for both patient and doctor than anything else. Many studies have been done over the years that show injections are stressful for everyone involved. Since we all know this, why is it that doctors just keep doing the same thing over and over?
Do you use topical anesthetic? If so, you’re probably taking a cotton swab of 20 percent benzocaine and placing it pretty close to where the target tissue is located. However, wet mucosa and the flow of saliva can quickly move or dilute the topical. If you really want good tissue penetration of the benzocaine, dry the tissue well with two-by-two gauze and keep the area dry while the topical sits in the area for two minutes. This greatly increases its effectiveness.
If you want even more profound topical anesthesia, invest in a topical referred to as EMLA. The abbreviation stands for Eutectic Mixture of Local Anesthetics. It’s a mixture of 2.5% prilocaine and 2.5% lidocaine in a cream. Originally developed for venipuncture, EMLA rapidly diffuses into mucosal tissue and provides profound topical anesthesia. It’s not inexpensive, but for many patients it’s a tremendous difference maker.
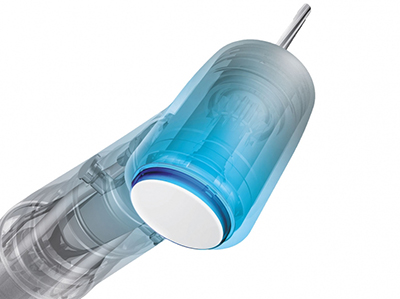
Another injection upgrade is The Wand®from Milestone Scientific. In addition to the pain of the needle stick, the other two uncomfortable parts of a dental injection are the pH difference of the anesthetic compared to the body and the pressure of the anesthetic fluid entering the body.
The Wand injects at a super slow rate. This means that the initial sting from the pH difference is decreased and the anesthetic diffuses into the tissue slowly instead of a 1.7-1.8cc bolus developing at the site of the injection due to a rapid injection technique.
Now I know all of you reading this are saying, “I give painless injections already and I inject super slowly!” I’m here to tell you that you do not. I once thought the same thing, but after switching to The Wand several years ago, it made a dramatic difference. Try it and you’ll see. It also helps that the needle handpiece looks like a translucent thin drinking straw and not some frightening shiny piece of stainless steel straight from a medieval dungeon.
The last discussion point of injections is the buffering of the anesthetic solution. There are at least two companies now on the market that offer ways of buffering anesthetic and both work well: Onpharma Company and Anutra Medical. Buffering anesthetic requires some extra steps and equipment, but it greatly decreases the sting and also increases the speed of anesthesia induction.
Electric handpieces
I switched exclusively to electric handpieces a few years ago and haven’t looked back. They produce incredible amounts of torque, which makes them darn near impossible to stall, even at low RPMs.
The increased torque can also allow the practitioner to use the handpiece at slower RPMs than air-driven handpieces, while accomplishing as much or even more. This generates lower decibels, which means the patient senses less handpiece noise, resulting in an overall better experience.
The high torque allows you to accomplish preparations with unbeatable precision faster than with air turbines. This means that treatment takes less time with the DC motor powered electric handpiece. There are at least two benefits that I feel are derived by this:
- Shorter appointment times for patients. Ask any anxious patient if he or she would like to have the appointment take longer and I can tell you what answer you’ll get. Being more efficient and requiring less time is a huge win for the patient.
- Benefit to your posture. The “clinical posture” that we place ourselves in during treatment takes a tremendous physical toll on the body. At some point during their careers, almost all full-time practitioners experience neck and back pain due to their clinical posture. Sometimes this damage/pain can become permanent and lead to disability. One of the easiest ways to prevent this is to spend less time in the posture.
By making appointments shorter by usuing electric handpireces, efficiency is a winner for the doctor as well. There are many good electric handpiece companies on the market. In my office, I use a mixture of Bien Air and KaVo electrics.
Digital caries detection
Hand in hand with the concept of efficiency and shorter appointments comes more accurate diagnosis. In case you haven’t heard, the sharp explorer diagnosis is dead and not even the best AED is going to bring it back.
Instead, the profession has moved on to visual, instead of exclusively tactile, diagnosis. Utilizing surgical scopes, intense clinical lighting and a variety of digital devices allows doctors to see decay at its earliest stages before the lesion either destroys or requires removal of extensive amounts of tooth structure to correct the situation.
Often this can be done with no anesthetic and small amounts of composite resin. Appointments for restoring these clinical situations are short, and many can be restored without the dreaded needle that all patients fear.
The devices are digital and produce images that can be shared with patients in a co-diagnosis environment. Being able to explain treatment and the reason behind it creates an environment in which the patient learns and appreciates the doctor’s focus on early diagnosis and minimally invasive restorations, allows the office to gain increased patient trust, and also provides opportunitites for internal marketing when patients tell friends, relatives and co-workers about their diagnostic and restorative appointments.
One of the most stressful things that doctors face is a terrified patient who requires extensive treatment. The more involved the treatment becomes, the greater the patient anxiety. By utilizing digital devices and more accurate diagnosis, patient and practitioner stress levels can be decreased.